January 26, 2023
Department of Labor announces enforcement guidance changes to save lives, target employers who put profit over safety
Seeks to hold employers to greater account for safety, health failures
WASHINGTON – The U.S. Department of Labor announced that its Occupational Safety and Health Administration has issued new enforcement guidance to make its penalties more effective in stopping employers from repeatedly exposing workers to life-threatening hazards or failing to comply with certain workplace safety and health requirements.
OSHA Regional Administrators and Area Office Directors now have the authority to cite certain types of violations as “instance-by-instance citations” for cases where the agency identifies “high-gravity” serious violations of OSHA standards specific to certain conditions where the language of the rule supports a citation for each instance of non-compliance. These conditions include lockout/tagout, machine guarding, permit-required confined space, respiratory protection, falls, trenching and for cases with other-than-serious violations specific to recordkeeping.
The change is intended to ensure OSHA personnel are applying the full authority of the Occupational Safety and Health Act where increased citations are needed to discourage non-compliance. The new guidance covers enforcement activity in general industry, agriculture, maritime and construction industries, and becomes effective 60 days from Jan. 26, 2023. The current policy has been in place since 1990 and applies only to egregious willful citations.
In a second action, OSHA is reminding its Regional Administrators and Area Directors of their authority not to group violations, and instead cite them separately to more effectively encourage employers to comply with the intent of the OSH Act.
“Smart, impactful enforcement means using all the tools available to us when an employer ‘doesn’t get it’ and will respond to only additional deterrence in the form of increased citations and penalties,” explained Assistant Secretary for Occupational Safety and Health Doug Parker. “This is intended to be a targeted strategy for those employers who repeatedly choose to put profits before their employees’ safety, health and wellbeing. Employers who callously view injured or sickened workers simply as a cost of doing business will face more serious consequences.”
These changes in enforcement guidance are important enforcement tools to help deter employers from disregarding their responsibilities to protect workers and ensure compliance with OSHA standards and regulations.
Existing guidance on instance-by-instance citations are outlined in the OSHA Field Operations Manual, and CPL 02-00-080, “Handling of Cases to be Proposed for Violation-by-Violation Penalties.”
Protecting Temporary Workers
Updated December 13, 2021
Employer Responsibilities to Protect Temporary Workers
To ensure that there is a clear understanding of each employer’s role in protecting employees, OSHA recommends that the temporary staffing agency and the host employer set out their respective responsibilities for compliance with applicable OSHA standards in their contract. Including such terms in a contract will ensure that each employer complies with all relevant regulatory requirements, thereby avoiding confusion as to the employer’s obligations.
Joint Responsibility
While the extent of responsibility under the law of staffing agencies and host employers is dependent on the specific facts of each case, staffing agencies and host employers are jointly responsible for maintaining a safe work environment for temporary workers – including, for example, ensuring that OSHA’s training, hazard communication, and recordkeeping requirements are fulfilled.
OSHA could hold both the host and temporary employers responsible for the violative condition(s) – and that can include lack of adequate training regarding workplace hazards. Temporary staffing agencies and host employers share control over the worker, and are therefore jointly responsible for temporary workers’ safety and health.
OSHA has concerns that some employers may use temporary workers as a way to avoid meeting all their compliance obligations under the OSH Act and other worker protection laws; that temporary workers get placed in a variety of jobs, including the most hazardous jobs; that temporary workers are more vulnerable to workplace safety and health hazards and retaliation than workers in traditional employment relationships; that temporary workers are often not given adequate safety and health training or explanations of their duties by either the temporary staffing agency or the host employer. Therefore, it is essential that both employers comply with all relevant OSHA requirements.
Both Host Employers and Staffing Agencies Have Roles
Both host employers and staffing agencies have roles in complying with workplace health and safety requirements and they share responsibility for ensuring worker safety and health.
A key concept is that each employer should consider the hazards it is in a position to prevent and correct, and in a position to comply with OSHA standards. For example: staffing agencies might provide general safety and health training, and host employers provide specific training tailored to the particular workplace equipment/hazards.
- The key is communication between the agency and the host to ensure that the necessary protections are provided.
- Staffing agencies have a duty to inquire into the conditions of their workers’ assigned workplaces. They must ensure that they are sending workers to a safe workplace.
- Ignorance of hazards is not an excuse.
- Staffing agencies need not become experts on specific workplace hazards, but they should determine what conditions exist at their client (host) agencies, what hazards may be encountered, and how best to ensure protection for the temporary workers.
- The staffing agency has the duty to inquire and verify that the host has fulfilled its responsibilities for a safe workplace.
- And, just as important: Host employers must treat temporary workers like any other workers in terms of training and safety and health protections.
When You’ve Been Fully Vaccinated
How to Protect Yourself and Others
People are considered fully vaccinated:
- 2 weeks after their second dose in a 2-dose series, like the Pfizer or Moderna vaccines, or
- 2 weeks after a single-dose vaccine, like Johnson & Johnson’s Janssen vaccine
If it has been less than 2 weeks since your shot, or if you still need to get your second dose, you are NOT fully protected. Keep taking all prevention steps until you are fully vaccinated.
COVID-19 vaccines are effective at protecting you from getting sick. Based on what we know about COVID-19 vaccines, people who have been fully vaccinated can start to do some things that they had stopped doing because of the pandemic.
We’re still learning how vaccines will affect the spread of COVID-19. After you’ve been fully vaccinated against COVID-19, you should keep taking precautions in public places like wearing a mask, staying 6 feet apart from others, and avoiding crowds and poorly ventilated spaces until we know more.
What’s Changed
If you’ve been fully vaccinated:
- You can gather indoors with fully vaccinated people without wearing a mask.
- You can gather indoors with unvaccinated people from one other household (for example, visiting with relatives who all live together) without masks, unless any of those people or anyone they live with has an increased risk for severe illness from COVID-19.
- If you’ve been around someone who has COVID-19, you do not need to stay away from others or get tested unless you have symptoms.
- However, if you live in a group setting (like a correctional or detention facility or group home) and are around someone who has COVID-19, you should still stay away from others for 14 days and get tested, even if you don’t have symptoms.
What Hasn’t Changed
For now, if you’ve been fully vaccinated:
- You should still take steps to protect yourself and others in many situations, like wearing a mask, staying at least 6 feet apart from others, and avoiding crowds and poorly ventilated spaces. Take these precautions whenever you are:
- In public
- Gathering with unvaccinated people from more than one other household
- Visiting with an unvaccinated person who is at increased risk of severe illness or death from COVID-19 or who lives with a person at increased risk
- You should still avoid medium or large-sized gatherings.
- You should still delay domestic and international travel. If you do travel, you’ll still need to follow CDC requirements and recommendations.
- You should still watch out for symptoms of COVID-19, especially if you’ve been around someone who is sick. If you have symptoms of COVID-19, you should get tested and stay home and away from others.
- You will still need to follow guidance at your workplace.
What We Know and What We’re Still Learning
- We know that COVID-19 vaccines are effective at preventing COVID-19 disease, especially severe illness and death.
- We’re still learning how effective the vaccines are against variants of the virus that causes COVID-19. Early data show the vaccines may work against some variants but could be less effective against others.
- We know that other prevention steps help stop the spread of COVID-19, and that these steps are still important, even as vaccines are being distributed.
- We’re still learning how well COVID-19 vaccines keep people from spreading the disease.
- Early data show that the vaccines may help keep people from spreading COVID-19, but we are learning more as more people get vaccinated.
- We’re still learning how long COVID-19 vaccines can protect people.
- As we know more, CDC will continue to update our recommendations for both vaccinated and unvaccinated people.
Until we know more about those questions, everyone — even people who’ve had their vaccines — should continue taking basic prevention steps when recommended.
Coronavirus Disease 2019 (COVID-19) Situation Summary
This is an emerging, rapidly evolving situation and CDC will provide updated information as it becomes available, in addition to updated guidance.
Updated March 12, 2020
Background
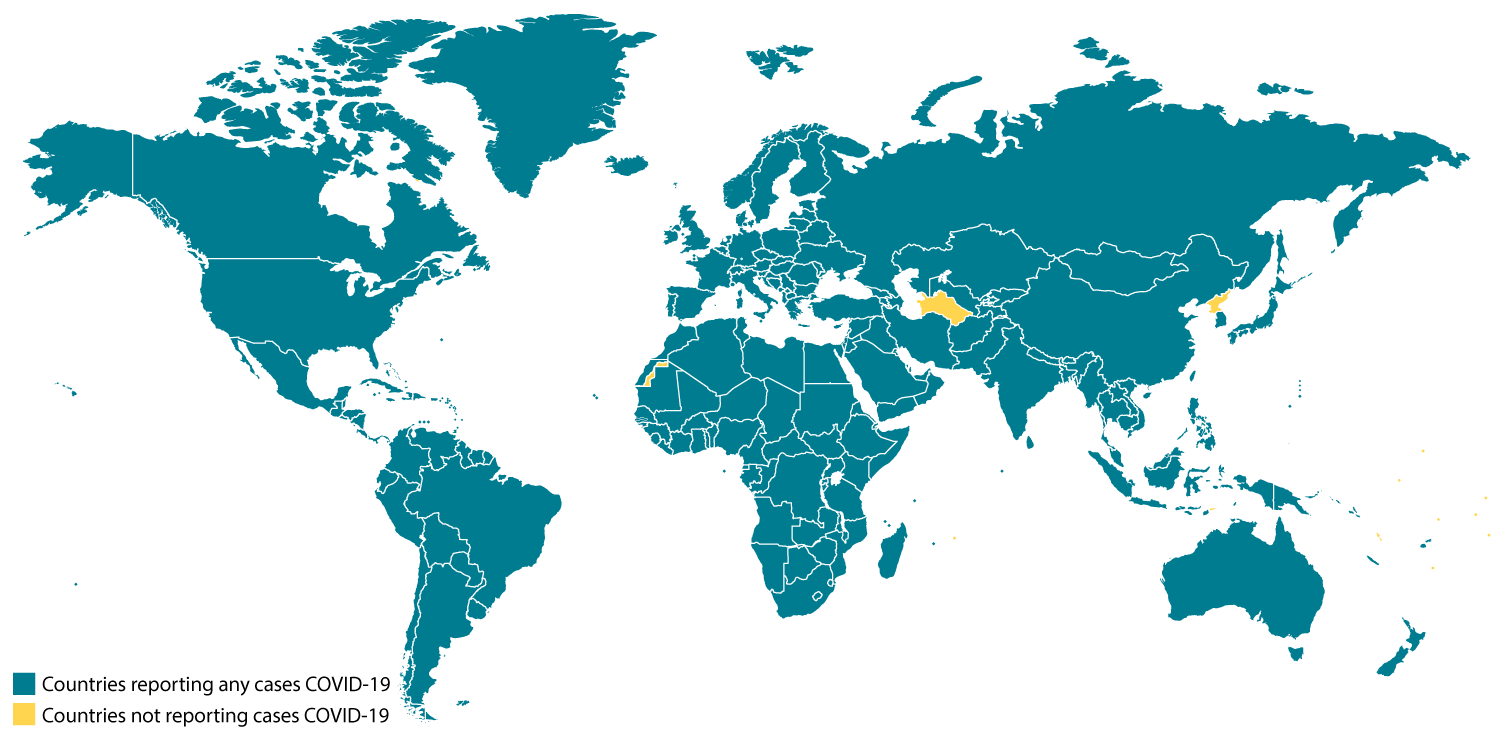
CDC is responding to an outbreak of respiratory disease caused by a novel (new) coronavirus that was first detected in China and which has now been detected in more than 100 locations internationally, including in the United States. The virus has been named “SARS-CoV-2” and the disease it causes has been named “coronavirus disease 2019” (abbreviated “COVID-19”).
On January 30, 2020, the International Health Regulations Emergency Committee of the World Health Organization declared the outbreak a “public health emergency of international concernexternal icon” (PHEIC). On January 31, 2020, Health and Human Services Secretary Alex M. Azar II declared a public health emergency (PHE) for the United States to aid the nation’s healthcare community in responding to COVID-19. On March 11, 2020 WHO publiclyexternal icon characterized COVID-19 as a pandemic.
Source and Spread of the Virus
Coronaviruses are a large family of viruses that are common in people and many different species of animals, including camels, cattle, cats, and bats. Rarely, animal coronaviruses can infect people and then spread between people such as with MERS-CoV, SARS-CoV, and now with this new virus (named SARS-CoV-2).
The SARS-CoV-2 virus is a betacoronavirus, like MERS-CoV and SARS-CoV. All three of these viruses have their origins in bats. The sequences from U.S. patients are similar to the one that China initially posted, suggesting a likely single, recent emergence of this virus from an animal reservoir.
Early on, many of the patients at the epicenter of the outbreak in Wuhan, Hubei Province, China had some link to a large seafood and live animal market, suggesting animal-to-person spread. Later, a growing number of patients reportedly did not have exposure to animal markets, indicating person-to-person spread. Person-to-person spread was subsequently reported outside Hubei and in countries outside China, including in the United States. Some international destinations now have apparent community spread with the virus that causes COVID-19, as do some parts of the United States. Community spread means some people have been infected and it is not known how or where they became exposed. Learn what is known about the spread of this newly emerged coronaviruses.
Severity
The complete clinical picture with regard to COVID-19 is not fully known. Reported illnesses have ranged from very mild (including some with no reported symptoms) to severe, including illness resulting in death. While information so far suggests that most COVID-19 illness is mild, a reportexternal icon out of China suggests serious illness occurs in 16% of cases. Older people and people of all ages with severe underlying health conditions — like heart disease, lung disease and diabetes, for example — seem to be at higher risk of developing serious COVID-19 illness.
Learn more about the symptoms associated with COVID-19.
COVID-19 Now a Pandemic
A pandemic is a global outbreak of disease. Pandemics happen when a new virus emerges to infect people and can spread between people sustainably. Because there is little to no pre-existing immunity against the new virus, it spreads worldwide.
The virus that causes COVID-19 is infecting people and spreading easily from person-to-person. Cases have been detected in most countries worldwide and community spread is being detected in a growing number of countries. On March 11, the COVID-19 outbreak was characterized as a pandemic by the World Health Organization (WHO)external icon.
This is the first pandemic known to be caused by the emergence of a new coronavirus. In the past century, there have been four pandemics caused by the emergence of novel influenza viruses. As a result, most research and guidance around pandemics is specific to influenza, but the same premises can be applied to the current COVID-19 pandemic. Pandemics of respiratory disease follow a certain progression outlined in a “Pandemic Intervals Framework.” Pandemics begin with an investigation phase, followed by recognition, initiation, and acceleration phases. The peak of illnesses occurs at the end of the acceleration phase, which is followed by a deceleration phase, during which there is a decrease in illnesses. Different countries can be in different phases of the pandemic at any point in time and different parts of the same country can also be in different phases of a pandemic.
There are ongoing investigations to learn more. This is a rapidly evolving situation and information will be updated as it becomes available.
Situation in U.S.
Different parts of the country are seeing different levels of COVID-19 activity. The United States nationally is currently in the initiation phases, but states where community spread is occurring are in the acceleration phase. The duration and severity of each phase can vary depending on the characteristics of the virus and the public health response.
- CDC and state and local public health laboratories are testing for the virus that causes COVID-19. View CDC’s Public Health Laboratory Testing map.
- More and more states are reporting cases of COVID-19 to CDC.
- U.S. COVID-19 cases include:
- Imported cases in travelers
- Cases among close contacts of a known case
- Community-acquired cases where the source of the infection is unknown.
- Three U.S. states are experiencing sustained community spread.
- View latest case counts, deaths, and a map of states with reported cases.
Risk Assessment
Risk depends on characteristics of the virus, including how well it spreads between people; the severity of resulting illness; and the medical or other measures available to control the impact of the virus (for example, vaccines or medications that can treat the illness) and the relative success of these. In the absence of vaccine or treatment medications, nonpharmaceutical interventions become the most important response strategy. These are community interventions that can reduce the impact of disease.
The risk from COVID-19 to Americans can be broken down into risk of exposure versus risk of serious illness and death.
Risk of exposure:
- The immediate risk of being exposed to this virus is still low for most Americans, but as the outbreak expands, that risk will increase. Cases of COVID-19 and instances of community spread are being reported in a growing number of states.
- People in places where ongoing community spread of the virus that causes COVID-19 has been reported are at elevated risk of exposure, with the level of risk dependent on the location.
- Healthcare workers caring for patients with COVID-19 are at elevated risk of exposure.
- Close contacts of persons with COVID-19 also are at elevated risk of exposure.
- Travelers returning from affected international locations where community spread is occurring also are at elevated risk of exposure, with level of risk dependent on where they traveled.
Risk of Severe Illness:
Early information out of China, where COVID-19 first started, shows that some people are at higher risk of getting very sick from this illness. This includes:
- Older adults, with risk increasing by age.
- People who have serious chronic medical conditions like:
- Heart disease
- Diabetes
- Lung disease
CDC has developed guidance to help in the risk assessment and management of people with potential exposures to COVID-19.
What May Happen
More cases of COVID-19 are likely to be identified in the United States in the coming days, including more instances of community spread. CDC expects that widespread transmission of COVID-19 in the United States will occur. In the coming months, most of the U.S. population will be exposed to this virus.
Widespread transmission of COVID-19 could translate into large numbers of people needing medical care at the same time. Schools, childcare centers, and workplaces, may experience more absenteeism. Mass gatherings may be sparsely attended or postponed. Public health and healthcare systems may become overloaded, with elevated rates of hospitalizations and deaths. Other critical infrastructure, such as law enforcement, emergency medical services, and sectors of the transportation industry may also be affected. Healthcare providers and hospitals may be overwhelmed. At this time, there is no vaccine to protect against COVID-19 and no medications approved to treat it. Nonpharmaceutical interventions will be the most important response strategy to try to delay the spread of the virus and reduce the impact of disease.
CDC Response
Global efforts at this time are focused concurrently on lessening the spread and impact of this virus. The federal government is working closely with state, local, tribal, and territorial partners, as well as public health partners, to respond to this public health threat.
CDC is implementing its pandemic preparedness and response plans, working on multiple fronts, including providing specific guidance on measures to prepare communities to respond to local spread of the virus that causes COVID-19. There is an abundance of pandemic guidance developed in anticipation of an influenza pandemic that is being adapted for a potential COVID-19 pandemic.
Highlights of CDC’s Response
- CDC established a COVID-19 Incident Management System on January 7, 2020. On January 21, CDC activated its Emergency Operations Center to better provide ongoing support to the COVID-19 response.
- The U.S. government has taken unprecedented steps with respect to travel in response to the growing public health threat posed by this new coronavirus:
- Foreign nationals who have been in China or Iran within the past 14 days cannot enter the United States.
- U.S. citizens, residents, and their immediate family members who have been in China or Iran within in the past 14 days can enter the United States, but they are subject to health monitoring and possible quarantine for up to 14 days.
- On March 11external icon, a similar policy was expanded to include 26 European countries for a period of 30 days.
- On March 8, CDC recommended that people at higher risk of serious COVID-19 illness avoid cruise travel and non-essential air travel.
- Additionally, CDC has issued the following additional specific travel guidance related to COVID-19.
- CDC has issued clinical guidance, including:
- On January 30, CDC published guidance for healthcare professionals on the clinical care of COVID-19 patients.
- On February 3, CDC posted guidance for assessing the potential risk for various exposures to COVID-19 and managing those people appropriately.
- On February 27, CDC updated its criteria to guide evaluation of persons under investigation for COVID-19.
- On March 8, CDC issued a Health Alert Network (HAN).
- On March 10, CDC issued updated infection control guidance for healthcare settings, including guidance on the use of personal protective equipment (PPE) during a shortage.
- CDC has deployed multidisciplinary teams to support state health departments case identification, contact tracing, clinical management, and public communications.
- CDC has worked with federal partners to support the safe return of Americans overseas who have been affected by COVID-19.

This is a picture of CDC’s laboratory test kit for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). CDC tests are provided to U.S. state and local public health laboratories, Department of Defense (DOD) laboratories and select international laboratories.
- An important part of CDC’s role during a public health emergency is to develop a test for the pathogen and equip state and local public health labs with testing capacity.
- CDC developed an rRT-PCR test to diagnose COVID-19.
- As of the evening of March 10, 79 state and local public health labs in 50 states and the District of Columbia have successfully verified and are currently using CDC COVID-19 diagnostic tests.
- Combined with other reagents that CDC has procured, there are enough testing kits to test more than 75,000 people.
- In addition, CDC has two laboratories conducting testing for the virus that causes COVID-19. CDC can test approximately 350 specimens per day.
- Commercial labs are working to develop their own tests that hopefully will be available soon. This will allow a greater number of tests to happen close to where potential cases are.
- CDC has grown the COVID-19 virus in cell culture, which is necessary for further studies, including for additional genetic characterization. The cell-grown virus was sent to NIH’s BEI Resources Repositoryexternal icon for use by the broad scientific community.
- CDC also is developing a serology test for COVID-19.
CDC Recommends
- Everyone can do their part to help us respond to this emerging public health threat:
- Individuals and communities should familiarize themselves with recommendations to protect themselves and their communities from getting and spreading respiratory illnesses like COVID-19.
- Older people and people with severe chronic conditions should take special precautions because they are at higher risk of developing serious COVID-19 illness.
- If you are a healthcare provider, use your judgment to determine if a patient has signs and symptoms compatible with COVID-19 and whether the patient should be testedexternal icon. Factors to consider in addition to clinical symptoms may include:
- Does the patient have recent travel from an affected area?
- Has the patient been in close contact with someone with COVID-19 or with patients with pneumonia of unknown cause?
- Does the patient reside in an area where there has been community spread of COVID-19?
- If you are a healthcare provider or a public health responder caring for a COVID-19 patient, please take care of yourself and follow recommended infection control procedures.
- If you are a close contact of someone with COVID-19 and develop symptoms of COVID-19, call your healthcare provider and tell them about your symptoms and your exposure. They will decide whether you need to be tested, but keep in mind that there is no treatment for COVID-19 and people who are mildly ill are able to isolate at home.
- If you are a resident in a community where there is ongoing spread of COVID-19 and you develop COVID-19 symptoms, call your healthcare provider and tell them about your symptoms. They will decide whether you need to be tested, but keep in mind that there is no treatment for COVID-19 and people who are mildly ill are able to isolate at home.
- For people who are ill with COVID-19, but are not sick enough to be hospitalized, please follow CDC guidance on how to reduce the risk of spreading your illness to others. People who are mildly ill with COVID-19 are able to isolate at home during their illness.
- If you have been in China or another affected area or have been exposed to someone sick with COVID-19 in the last 14 days, you will face some limitations on your movement and activity. Please follow instructions during this time. Your cooperation is integral to the ongoing public health response to try to slow spread of this virus.
Other Available Resources
The following resources are available with information on COVID-19
January 2020
The Top Occupational Safety and Health Issues for 2020: An Employer’s Guide
While forces affecting the workplace change rapidly—an aging workforce, new work arrangements, and state adoption of medical and recreational marijuana laws—regulatory changes move at a slower pace.

valeriagalindo / Shutterstock.com
The National Institute for Occupational Safety and Health (NIOSH) usually is at the forefront of workplace safety and health developments. NIOSH Director John Howard, MD, this fall unveiled a new “Future of Work” initiative.
The initiative at several units of NIOSH is looking at issues such as:
- The aging workforce;
- Shifting employment relationships like contingent or “gig” employment; and
- Uncertainty about how best to manage new technologies like artificial intelligence, robotics, and 3D printing entering the workplace.
NIOSH researchers are looking at issues that include particulates and volatile organic compounds emitted by 3D printers, rapid growth in fields like health care, and new occupations like solar photovoltaic installer and wind turbine service technician.
OSHA Rulemakings
Rulemaking at OSHA has slowed but not stopped during the Trump administration. The agency has made a few attempts at deregulation, mostly to address a last-minute Obama administration rulemaking for beryllium exposures.
After an effective date freeze and delayed enforcement of the revised beryllium standards, OSHA began enforcing provisions of the general industry standard on March 11, with enforcement of the engineering controls in the general industry standard starting March 10, 2020.
OSHA decided to implement ancillary provisions of the construction and shipyard standards it had proposed revoking, concluding that the provisions were not duplicated in other construction and shipyard standards.
However, the agency has not finished its work on beryllium regulation. It proposed amending definitions used in the construction and shipyards standards and removing certain provisions for hygiene areas and practices. It also would revise provisions for methods of compliance, respiratory protection, personal protective equipment (PPE), housekeeping, medical surveillance, communication of hazards, and recordkeeping.
While the agency abandoned an Obama-era proposal to remove a single word from the control of hazardous energy, or lockout/tagout, standard that many employers feared would broaden the scope of the standard, OSHA did decide to revisit the standard.
The agency asked for public comment on two changes to the standard it is considering:
- Allowing the use of control circuit-type devices while equipment or machines are being maintained or serviced; and
- Amending the general industry standard to address hazardous energy control for new robotics technologies.
OSHA has provided no update on any further rulemaking action on lockout/tagout.
A push for more workplace safety and health regulation likely will come from outside the agency. The American Society of Safety Professionals (ASSP) advocated for legislation extending OSHA’s authority to federal, state, and local government employment and another bill requiring the agency to establish a federal workplace violence prevention standard.
Six- or Seven-Figure OSHA Penalties
While some activists had predicted a Trump administration Labor Department would gut OSHA enforcement, the agency has continued to seek six-figure and even seven-figure penalties.
OSHA cited a Maine roofing contractor for 17 egregious willful, repeat, and serious workplace safety violations, seeking nearly $1.8 million in penalties.
The agency has proposed high-dollar penalties in several other cases:
- $724,380 in penalties for a Moraine, Ohio, glass manufacturer;
- $687,619 in penalties for two construction contractors at the Port of Wilmington, Delaware;
- $413,370 in penalties for a Lebanon, Missouri, barrel maker;
- $287,212 in penalties for a Hauppauge, New York, fabric-care product manufacturer; and
- $236,089 in penalties for a Pleasantville, New Jersey, produce wholesaler.
Employers can expect to see more six-figure penalties under OSHA’s new enforcement weighting system that emphasizes inspections for four construction industry hazards.
The agency assigns an Enforcement Unit (EU) measure for various inspections. OSHA heavily weighted inspections during the Obama administration for ergonomics, process safety management, and workplace violence hazards. The new enforcement weighting system de-emphasizes inspections for ergonomics and workplace violence but prioritizes inspections for:
- Caught-in or -between hazards,
- Electrical hazards,
- Fall hazards, and
- Struck-by hazards.
Citations for fall hazards resulted in some of OSHA’s largest penalties this year. Agency compliance safety and health officers (CSHOs) now have greater incentive to pursue these inspections.
Aging Workforce
Employment of workers aged 65 or older has grown by 117% in a span of 20 years, according to the Labor Department’s Bureau of Labor Statistics (BLS), and one in four American workers will be over the age of 55 by 2020.
While older workers are less likely to become injured, their injuries are more severe and sometimes fatal.
The BLS has found a significant correlation between worker age and both the number and the rate of fatal workplace injuries.
The highest fatal injury rate now is among workers aged 65 years and over. They accounted for 775 deaths in 2017 at a rate of 10.3 workers per 100,000. Workers aged 65 or over accounted for 15% of fatally injured workers—an all-time high in the 26-year history of the BLS’s Census of Fatal Occupational Injuries.
Heat Stress
Each summer is hotter than the last. National Air and Space Administration data show 18 of the past 19 years have been the hottest on record.
Expect OSHA to cite more employers for violations of the Occupational Safety and Health Act’s General Duty Clause. And enforcement cases are not limited to Sun Belt states. OSHA recently cited a utility-pole service provider in the heat-related death of a worker at a site in Inman, Nebraska.
Expect legislators and activists to continue pushing for OSHA to adopt a heat stress standard. Public Citizen and 111 other groups urged the secretary of Labor and head of OSHA to establish a federal standard for protecting workers from heat stress.
Rep. Judy Chu (D-CA) and 27 cosponsors introduced a bill in the House of Representatives this summer requiring OSHA to issue a proposed heat stress standard within 2 years and a final regulation within 42 months. The federal standard would have to be at least as effective as the most stringent state standard and include provisions for hydration and paid rest breaks, medical surveillance, and recordkeeping.
Fatigue
The National Safety Council (NSC) estimates a typical employer with 1,000 employees can expect to lose more than $1 million a year due to fatigue:
- $272,000 due to absenteeism,
- $776,000 due to “presenteeism” (employees who are at work but not fully functional), and
- $536,000 in healthcare costs.
The NSC and researchers at Brigham and Women’s Hospital in Boston developed the “NSC Fatigue Cost Calculator” to estimate the cost of sleep deficiency for individual businesses.
Fatigue has been cited as a factor in some of the biggest industrial accidents in history, including the 2005 BP Texas City oil refinery explosion, 2009 Colgan Air Crash, and 2010 Deepwater Horizon oil spill.
Fatigue also is a leading cause in motor vehicle crashes, and even nonfatal injuries can be serious. While the median number of days away from work for most workplace injuries is 8 days, the median for roadway incidents is 10.
The ASSP began studying the use of body sensors to help detect signs of fatigue and alert supervisors to the need for intervention. Researchers found the common root causes of fatigue were lack of sleep, shift schedule, and work stress. Wearable sensors monitoring body movements can detect the starting point of fatigue. Wearable sensors can detect physical fatigue in a number of different occupational settings, and researchers suggested manufacturing-sector employers could benefit from investing in data-driven assessments to prevent occupational injury.
However, employees and labor unions could challenge the adoption of body sensor technology.
The American Industrial Hygiene Association (AIHA) supports collecting and analyzing large amounts of data from body sensors to better protect workers. The group called for significant increases in funding for research and development of sensors to detect workers’ exposures to biological, chemical, physical, and radiological hazards.

Canna Obscura / Shutterstock.com
Cannabis
Safety problems posed by worker impairment will plague employers as more states pass medical and recreational cannabis/marijuana laws.
Illinois became the 11th state to legalize recreational use of marijuana. Now, 34 states and Washington, D.C., have legalized either medical or recreational marijuana use. Illinois’s law goes into effect January 1. Several bills to decriminalize, reclassify, or legalize marijuana also have been introduced in the U.S. Congress.
Employers have good reason for concern. Positive drug test results for transportation and warehousing workers increased by double digits between 2015 and 2017, according to laboratory testing firm Quest Diagnostics.
Six industry sectors saw year-over-year increases in positive results for marijuana of least 20%—transportation and warehousing, other services, construction, wholesale trade, manufacturing, and accommodation and food services.
There is no test yet that measures the degree of impairment caused by various levels of tetrahydrocannabinol (THC).
While the impacts of various blood alcohol levels are well understood, the science behind marijuana impairment is not as well defined. In the absence of any reliable impairment testing, the AIHA and NSC both have advocated for zero-tolerance policies for workers in safety-sensitive positions.
The NSC has pointed out that an increase in motor vehicle accidents involving THC occurs in states after implementation of medical or recreational marijuana laws. The American College of Occupational and Environmental Medicine (ACOEM) also released a policy statement cautioning that marijuana interferes with safety performance in the workplace.